Infectious diseases exact a high toll on sub-Saharan Africa. COVID aside – which has caused an estimated 173 988 deaths in Africa to date – TB, malaria and HIV continue to drive mortality rates. In 2021, Africa accounted for 23% of new TB cases worldwide; 95% of malaria cases and 96% of malaria deaths (with children under five accounting for about 80% of all malaria deaths); and by far the highest share of global total new HIV infections (860 000), with about 66% of the total number of people living with HIV located in sub-Saharan Africa.
As the COVID pandemic recedes, TB is once again the deadliest disease in Africa. Malaria cases appear to have stabilised, and while HIV infection rates continue to decline in some regions, Africa is still the epicentre for global infections.
Yet these diseases, whose prevalence is inextricably linked to poor socio-economic conditions, are set to be eclipsed by an entirely different category of illness.
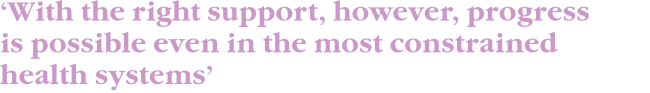
The WHO reports that non-communicable diseases (NCDs) are about to become the leading causes of death in sub-Saharan Africa by 2030 – exerting additional pressure on the region’s already-strained treatment and care services.
NCDs – also known as chronic diseases – refer to diseases that are not transmissible and are typically caused through behavioural, environmental and/or congenital conditions. Cardiovascular disease, cancer, hypertension, diabetes, sickle cell and Alzheimer’s disease are all examples of NCDs.
NCDs were responsible for 37% of deaths in Africa in 2019, rising from 24% in 2000, ‘largely due to weaknesses in the implementation of critical control measures including prevention, diagnosis and care’, according to the WHO.
Matshidiso Moeti, WHO regional director for Africa, has voiced concern that premature deaths from NCDs are rising among people younger than 70 years – intimating that external conditions, rather than old age, are the cause.
So what’s driving this alarming rise? Well, the COVID-19 pandemic didn’t help, says the WHO. ‘About 80% of countries in Africa reported disruption to at least one health service against non-communicable disease between May and September 2021. Countries are striving to restore services, although many have not yet been fully re-established.’
The causes of NCDs in Africa may overlap with, but are unlikely to mirror, those of developed nations. Seventy-seven percent of all NCD deaths are in low- and middle-income countries, suggesting poor socio-economic conditions play a role, such as malnutrition, poor oral health and poor air quality; whereas NCD risk factors particular to developed nations are more likely to be associated with affluence or urbanisation, such as greater consumption of saturated fats, cholesterol and dietary calories. Consumption of cigarettes, alcohol, poor nutrition and decreased physical activity are risk factors common to most populations.

‘The Lancet Commission on Reframing Non-communicable Diseases and Injuries for the Poorest Billion showed that NCDs are a major endemic cause of suffering and death for rural populations in Africa,’ says Gene Bukhman, co-chair of the NCDI Poverty Network steering committee and associate professor at Harvard Medical School. ‘These NCDs include an extremely diverse set of conditions ranging from Type 1 diabetes, rheumatic heart disease, and sickle cell disease to childhood cancer, and severe mental illness. This is due to the persistence of risk factors directly related to poverty such as […] lack of access to healthcare.’
Anne Kamau, deputy director of the African Research Universities Alliance Centre of Excellence for NCDs at the University of Nairobi, Kenya, elaborates. ‘NCDs are broad and cut across individuals’ lifespan. They vary according to demographic factors – age, gender, social class, social-economic status; geographical factors – rural and urban; within urban settings – low-income, middle-income, and upper-income areas. They are also linked to environmental factors, for instance expo-sure to air pollution, social and cultural environments that individuals live in, and several other factors.
‘Wealth and poverty, as well as urbanisation all contribute to the rising NCDs problem [in Africa]. While the rising middle class has higher obesity levels, partly due to sedentary lifestyle, this is also a result of ineffective planning to address the lifestyle needs of individuals,’ says Kamau.
‘In countries with better health outcomes, walking and cycling are prioritised, as well as use of travel modes that integrate walking. Hence, urbanisation is not the problem, but how well urban systems are designed to respond to the health needs of citizens, and through provision of enabling infrastructure.
‘With the right infrastructure and public engagement/education, individuals have the capacity to adopt healthier lifestyles. With poverty, this becomes a problem especially with regard to access to health services that would promote early detection and prevention of NCDs,’ she says.
‘The state of health services in most sub-Saharan African countries is such that individuals seek care mostly when sick, and for the poor, this is likely when NCDs like cancer, hypertension and related health challenges are at an advanced stage. The challenge therefore is not just poverty, but lack of inclusive healthcare systems. Individuals most affected by poverty live in rural areas and in the urban informal settlements.’
The urgency of taking action is not lost on authorities. In April 2022, a landmark meeting in Ghana saw heads of state and health leaders sitting down to find ways of accelerating progress against NCDs, emphasising the double burden of both infectious and non-communicable diseases driving inequality and increasing pressure on health systems and the demand for scarce resources in Asian and African countries.
Then, in May, the Africa Centre for Disease Control and Prevention initiated the Non-Communicable Diseases, Injuries and Mental Health strategy for 2022–2026. The strategy is designed to boost investment in African health systems and promote multi-sectoral collaboration.
Interestingly, both of the above-mentioned agendas acknowledged the importance of empowering communities, which echoes the call of several health researchers for the decentralisation of health services.
Diabetes and hypertension care in a rural district setting can be safely delivered by nurses in community clinics adhering to a shared care protocol, according to one study. Another found that the government of Rwanda was able to scale a nurse-led outpatient NCD programme to all first-level hospitals with good fidelity, feasibility and penetration.
Bukhman agrees. ‘It is absolutely a good idea. One example of this kind of promising initiative is the Package of Essential NCD Interventions Plus [PEN-Plus]. PEN-Plus is a strategy to train nurses to manage severe chronic NCDs such as Type 1 diabetes, rheumatic and congenital heart disease, and sickle cell disease close to where people live rather than at big hospitals in urban centres. This approach is already being introduced in 11 countries on the continent, and this year the 47 countries of the World Health Organisation’s African region resolved to achieve high-levels of PEN-Plus coverage by 2030.’
The problem of non-communicable diseases is very broad, adds Bukhman. ‘Often what’s needed is to break it down into groups of related services that can have an impact on multiple diseases. That’s what we call integration science. Both treatment and prevention are important. But it’s important not to forget that many of the conditions that we are talking about are not necessarily preventable – think about childhood cancer, for example – and so it’s important to be very clear what disease you are addressing.’
He says that probably the biggest problem is, ‘not surprisingly’, financing. ‘We have shown that cost of implementing PEN-Plus strategies is on the order of US$0.50 to US$1 per person. Low-income countries in the region are already stretched. In many cases this money will have to come from philanthropy until the overall economic situation improves. With the right support, however, progress is possible even in the most constrained health systems.’